CASE REPORT |
https://doi.org/10.5005/jp-journals-10079-1083 |
An Unusual Presentation of Buckling Collapse Type of Kyphoscoliosis in Neurofibromatosis: A Case Report
1-3 Spine Surgery, SKS Hospital, Salem, Tamil Nadu, India
Corresponding Author: Vishnu PCS, Spine Surgery, SKS Hospital, Salem, Tamil Nadu, India, Phone: +91 8122420061, e-mail: sachumoogly@gmail.com
ABSTRACT
Spinal deformities such as kyphoscoliosis are the most common skeletal abnormalities in neurofibromatosis. Dystrophic type of spine deformities mostly progress over time, leading to significant morbidity and mortality to the patient, hence early surgical intervention is indicated. Here we are presenting 22 years, male with dystrophic type thoracic kyphoscoliosis, who presented unusually with worsening of thoracic myelopathy after halo gravity traction (HGT), to help in the subsequent surgical correction. In literature, for buckling collapse type of kyphosis, HGT is advised and there are very few reports of worsening of neurology with the application of HGT. Hence this case report will add to the literature of treatment of severe dystrophic spinal deformities in neurofibromatosis.
How to cite this article: V V, Goyal N, C S VP. An Unusual Presentation of Buckling Collapse Type of Kyphoscoliosis in Neurofibromatosis: A Case Report. J Orth Joint Surg 2022;4(2):81-84.
Key messages: Dystrophic type of spinal deformities in neurofibromatosis progress without further intervention and worsening of neurology with halo gravity traction can be an unexpected consequence while treating these patients
Source of support: Nil
Conflict of interest: None
Keywords: Buckling collapse type, Dystrophic type, Halo gravity traction, Neurofibromatosis, Thoracic myelopathy
INTRODUCTION
In Neurofibromatosis, spinal deformities are two types, that is, dystrophic type and non-dystrophic type.1-3 Dystrophic type of deformity mostly progress with time, which leads to significant morbidity and mortality to the patient. Early surgical intervention is indicated for dystrophic curves to avoid progression of the deformity and neurological deterioration.3-6 The main aim of the surgery is to stop the progression of the deformity, improving cardiopulmonary reserve, avoiding the effects of restrictive lung disease, and to improve quality of life.6,7,9,10
Halo gravity traction (HGT) is used preoperatively in cases of complex spinal deformities to help in later surgical correction.11,12 The increase of traction weights gradually allows for stretching of the spinal column which helps to reduce the risk of neurologic injury during the definitive surgical correction.13-15
Although HGT was shown to be well-tolerated method to provide preoperative correction, we report a case of neurologic deterioration during HGT in a 22-year-old patient with severe kyphoscoliosis and discussed the treatment modality which aided in the functional recovery of the patient.
Case Description
A 22-year-old male, known case of Neurofibromatosis, presented with deformity of the back since 7 years of age, gradually progressive and associated with low back pain. He had no significant past medical or surgical history. On examination, Plexiform Neurofibroma was seen arising at the apex of the curve. He had left thoracic scoliosis with hyperkyphosis, anterior chest protuberance (Fig. 1). Motor power was normal in both upper and lower limbs with exaggerated deep tendon reflexes and clonus bilaterally, suggestive of early myelopathy. He is ambulant independently, with a normal gait (Video 1).
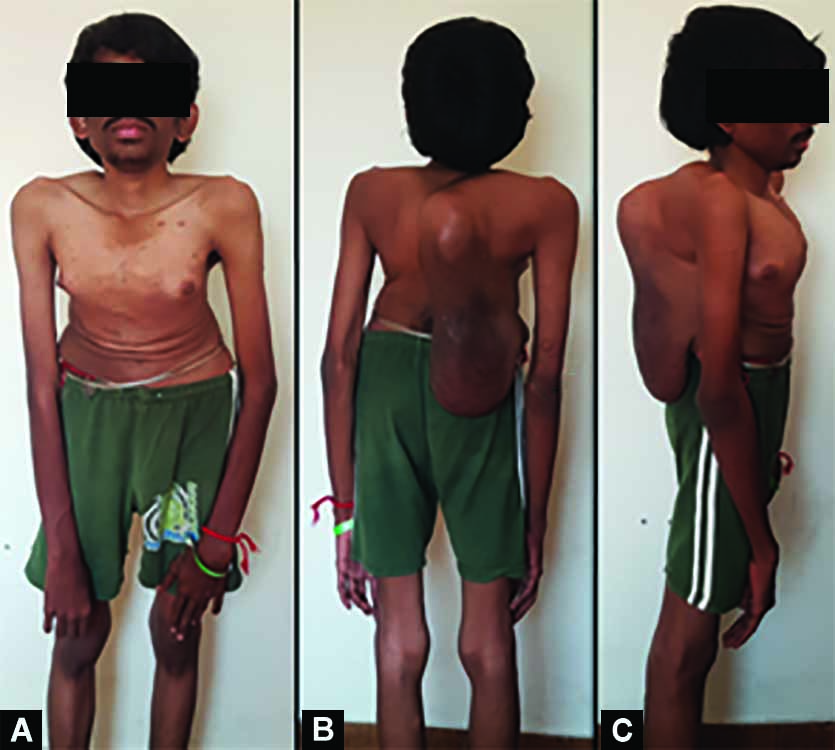
Fig.1: Plexiform neurofibroma arising at the apex of the deformity
Plain X-rays showed severe thoracic kyphoscoliosis with >180° of scoliosis deformity (Fig. 2). Computed tomography with 3D reconstruction showed the buckling collapse type of kyphosis8 (Fig. 3). In magnetic resonance imaging, the spinal cord was draped and stretched over the apex of the deformity at T8–10 (Fig. 4). The baseline pulmonary function test showed restrictive lung disease with a FVC of 39% (reference, 2.82; predicted, 1.11) and forced expiratory volume in 1 second of 41% (reference, 2.55; predicted, 1.05) for his weight of 37 kg and height of 143 cm.

Fig. 2: AP and lateral X-rays showing a severe thoracic kyphoscoliosis with >180° of 3-dimensional deformity

Fig. 3: Three-dimensional computed tomography showing the bayoneted nature of the kyphosis

Fig. 4: T2W MRI sequence showing the draped spinal cord across the apex
We planned for preoperative HGT, up to the recommended traction weight of 15 kg (52% body weight).13-15 Over the course of the first 15 days, he reached his goal traction weight of 15 kg (Fig. 5). During week 3, he started developing unsteadiness of gait and difficulty in walking with clonus and exaggerated deep tendon reflexes with plantar extensor response, suggestive of worsening of myelopathy (Video 2). In check X-ray of full spine with and without traction, there was no correction happening at the apex of the curve, instead, the proximal portion of the curve was found stretched alone, which might have caused more stretching of the cord over the apex of the curve and worsening of myelopathy (Fig. 6). Immediately traction was released, but there is no improvement of neurology. Because of the rigid nature of the curve and progressive compression and worsened neurology, which was not improved after releasing of traction, it was planned for decompression of the cord and anterior fusion procedure to avoid further worsening.

Fig. 5: Clinical picture showing the halogravity traction at 15 kg

Fig. 6: Lateral X-rays without and with traction showing the stretching of proximal portion of curve alone
After thorough preoperative evaluation, he underwent spinal cord decompression from T7–T10 with internal gibbectomy plus anterior reconstruction using rectangle cage and cylindrical cage with bone graft under neuromonitoring. After exposure, defining the dysplastic anatomy, T8–T11 pedicles, on the concavity, on which the cord was found stretched were removed to the pedicle-body junction and the spinal cord was decompressed. The buckling curve at T8–T11 was exposed anteriorly through extracavitary approach and was packed with autogenous bone and rectangle and cylindrical cages to prevent further collapse of the curve.
Postoperatively he was monitored in the ICU and ambulated with walker support from first postoperative day. Postoperative standing films showed adequate placement of the cages (Fig. 7). At 6-month follow-up, he has normal power in lower extremities with signs of improvement clinically. Follow-up radiographs showed instrumentation to be in satisfactory position with no further buckling of the curve. Informed written consent was obtained from the patient for the publication of the case report.

Fig.7: Postoperative AP and lateral X-rays showing anterior cages and bone graft
DISCUSSION
In Neurofibromatosis, dystrophic type of curves are known to progress, leading to significant morbidity and mortality to the patient, hence early surgical intervention is indicated. The use of HGT helps in the partial preoperative correction of rigid spinal deformities.13-15 This leads to increase pulmonary function, improve overall tolerance of the patient for a complex definitive surgery, and decrease the need for complex procedures like vertebral column resections, which are associated with higher complication rates.5,7,9
Koller et al.11 in their study in 10 patients with neurologic deficits preoperatively, found that with the application of HGT, all patients had improvement in spasticity, hyperreflexia, and motor/sensory symptoms. In conclusion they found that patients on HGT improves clinically especially in the setting of sick spinal cord that is stretched over the apex of a severe kyphoscoliosis deformity.
Neurologic complications after HGT are extremely rare and have been reported to be 1% in a recent systematic review and meta-analysis by Yang et al.13 Overall traction-related complications were common at 22% (43 non-neurologic traction-related complications in 197 patients across 10 articles), they did find three patients (of 292 patients in 13 studies) who experienced neurologic deficits in HGT.
Bouchoucha et al.15 reported a patient who presented with hyperreflexia, clonus, spasticity, and mild weakness in his bilateral distal lower extremities after HGT. This suggests that in some patients who had a preoperative neurologic deficit, the spinal cord has less tolerance even for gradual correction in HGT. The development of neurologic deficits after traction shows that the spinal cord is already compromised and there is dysfunction due to tension at the apex and reduction in the normal blood supply. Our patient also had the added compressive effects, which leads to the worsening of myelopathy features. In this case report, we discussed the development of neurologic deficits during HGT, which is a rare occurrence.
CONCLUSION
HGT is a safe method for the preoperative partial correction of severe rigid spinal deformity. We need to have a high index of suspicion for development of neurological deficits or worsening of neurology should be kept in mind, especially in case of severe decompensated Kyphoscoliosis such as in Neurofibromatosis.
Video 1: Before HGT application
Video 2: Unsteady gait after halo gravity traction application
REFERENCES
1. Calvert PT, Edgar MA, Webb PJ. Scoliosis in neurofibromatosis. The natural history with and without operation. J Bone Joint Surg Br 1989;71(2):246–251. DOI: 10.1302/0301-620X.71B2.2494186
2. Akbarnia BA, Gabriel KR, Beckman E, et al. Prevalence of scoliosis in neurofibromatosis. Spine (Phila Pa 1976) 1992;17(8 Suppl):S244–S248. DOI: 10.1097/00007632-199208001-00005
3. Funasaki H, Winter RB, Lonstein JB, et al. Pathophysiology of spinal deformities in neurofibromatosis. An analysis of seventy-one patients who had curves associated with dystrophic changes. J Bone Joint Surg Am 1994;76(5):692–700. DOI: 10.2106/00004623-199405000-00010
4. Tsirikos AI, Saifuddin A, Noordeen MH. Spinal deformity in neurofibromatosis type-1: diagnosis and treatment. Eur Spine J 2005;14(5):427–439. DOI: 10.1007/s00586-004-0829-7
5. Park YS, Hyun SJ. Spinal deformity in neurofibromatosis: classification and management. Eur Spine J 2005;14(5):427–439. DOI: 10.1007/s00586-004-0829-7
6. Rhodes SD, Zhang W, Yang D, et al. Dystrophic spinal deformities in a neurofibromatosis type 1 murine model. PloS one 2015;10(3):e0119093. DOI: 10.1371/journal.pone.0119093
7. De Barros AGCD, Le Silva LECT, Ponte JA, et al. Correction of severe dystrophic scoliosis in neurofibromatosis 1 with posterior vertebral column resection in multiple levels. Coluna/Columna 2019;18(3):187–191. DOI: 10.1590/S1808-185120191803195306
8. Rajasekaran S, Rajoli SR, Aiyer SN, et al. A classification for kyphosis based on column deficiency, curve magnitude, and osteotomy requirement. J Bone Joint Surg Am 2018;100(13):1147–1156. DOI: 10.2106/JBJS.17.01127
9. Cai S, Tian Y, Qiu G, et al. Neurofibromatosis type 1 with severe dystrophic kyphosis: surgical treatment and prognostic analysis of 27 patients. Orthop Surg 2020;12(6):1923–1940. DOI: 10.1111/os.12848
10. Kalidindi KK, Sath S, Sharma J, et al. Management of severe rigid scoliosis by total awake correction utilizing differential distraction and in situ stabilization. Interdiscip Neurosurg 2020;21:100778. DOI: 10.1016/j.inat.2020.100778
11. Koller H, Zenner J, Gajic V, et al. The impact of halo-gravity traction on curve rigidity and pulmonary function in the treatment of severe and rigid scoliosis and kyphoscoliosis: a clinical study and narrative review of the literature. Eur Spine J 2012;21(3):514–529. DOI: 10.1007/s00586-011-2046-5
12. Garabekyan T, Hosseinzadeh P, Iwinski HJ, et al. The results of preoperative halo-gravity traction in children with severe spinal deformity. J Pediatr Orthop B 2014;23(1):1–5. DOI: 10.1097/BPB.0b013e32836486b6
13. Yang C, Wang H, Zheng Z, et al. Halo-gravity traction in the treatment of severe spinal deformity: a systematic review and meta-analysis. Eur Spine J 2017;26(7):1810–1816. DOI: 10.1007/s00586-016-4848-y
14. Rinella A, Lenke L, Whitaker C, et al. Perioperative halo-gravity traction in the treatment of severe scoliosis and kyphosis. Spine (Phila Pa 1976) 2005;30(4):475–482. DOI: 10.1097/01.brs.0000153707.80497.a2
15. Bouchoucha S, Khelifi A, Saied W, et al. Progressive correction of severe spinal deformities with halo-gravity traction. Acta Orthop Belg 2011;77(4):529–534. PMID: 21954764.
________________________
© The Author(s). 2022 Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (https://creativecommons.org/licenses/by-nc/4.0/), which permits unrestricted use, distribution, and non-commercial reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.